When you’re diagnosed with multiple sclerosis (MS), there’s a lot to learn. You find out that MS is a chronic neurological disorder that causes lesions within the central nervous system. The lesions form when the immune system mistakenly attacks myelin, the layer of insulation surrounding nerve fibers in the brain and spinal cord. These lesions interrupt nerve signals between the brain and the rest of the body. It’s a communication problem. This results in a variety of potential symptoms, depending on the location of the lesions.
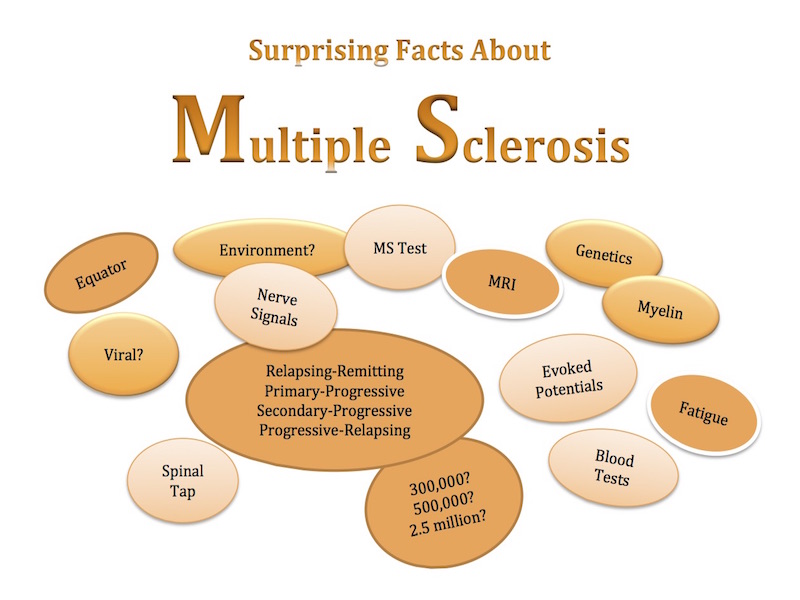
We know that women get MS at a higher rate than men. You can be diagnosed at any age, but it’s most likely to happen when you’re between the ages of 20 and 50. We know it’s not contagious and that it’s a chronic illness. Researchers have uncovered a lot of new information about the disease in recent decades, but much mystery remains. Some of what we do know and some of what we don’t know about MS may surprise you:
1. We don’t know how many people have MS.
We’re not sure how many people in the United States are living with MS. That’s because there there’s no national registry and doctor’s aren’t required to report new cases of MS to the Centers for Disease Control and Prevention (CDC) or any other agency. Estimates range from 350,000 to 500,000. For some people, symptoms are mild, or they come and go, making diagnosis difficult, so the actual number of cases may be much higher. Worldwide, it is estimated that more than 2.5 million people have MS.
2. We don’t know what causes MS.
Researchers have come a long way, but we still don’t understand exactly what causes MS. It’s not inherited, but there does seem to be a genetic predisposition for developing MS. We do know that the incidence of MS rises as you get farther from the equator. In MS, the immune system mistakenly attacks myelin, the protective substance that surrounds nerve fibers. Exactly what triggers that response is unclear. Some avenues of research include viruses, infectious agents, and other environmental factors.
3. There’s no test for MS.
There’s no simple way to diagnose MS, no single test that can give you a definitive answer. It takes patient history, neurological exam, and a series of tests to reach a diagnosis. Because symptoms of MS are similar to those of other neurological disorders, some tests are performed to rule those out. Diagnostic testing may include:
- magnetic resonance imaging (MRI) of the head and spine to view old lesions and active lesions in the central nervous system
- blood tests to rule out a variety of other disorders
- evoked potentials to measure how your nervous system responds to stimulation
- visual evoked potentials
- lumbar puncture (spinal tap) to search for inflammatory cells and rule out certain infections and other illnesses
To arrive at the diagnosis of MS, your doctor must be able to identify two distinct areas of damage in the central nervous system, conclude that the damage happened at different times, and rule out all other possibilities.
4. There’s more than one type of MS.
You can’t judge one person’s MS by another’s because symptoms vary a great deal and range from a mild course to severely debilitating. There are also four main types of MS:
- Relapsing-remitting MS (RRMS), the most common type at diagnosis, has clearly defined attacks that come and go. They may last from a few days to a month or more. In periods of remission, the disease does not progress. During that time, you may have residual symptoms or complete recovery.
- Primary-progressive MS (PPMS) has no clear relapses or remission. There’s a steady disease progression from the start.
- Secondary-progressive MS (SPMS) gets its start as RRMS, but eventually changes to the progressive form.
- Progressive-relapsing MS (PRMS) is progressive from the beginning, but there are also distinct relapses.
5. Fatigue is often the most debilitating symptom of MS.
There are a lot of symptoms of MS, and many of them are debilitating. Fatigue is one of those “invisible” symptoms that can really pack a punch. For people with immune system diseases, fatigue takes on a whole new meaning. It’s not feeling tired. It’s not being a little sleepy. A full night’s sleep does not cure this type of fatigue. It’s a down-to-your-bones overwhelming exhaustion that makes it hard to move and tackle simple tasks. Fatigue of this nature can become disabling. People who live with chronic fatigue are often labeled as lazy or antisocial. This misunderstanding can create an emotional burden.
Despite the many unknowns, since the advent of the MRI, doctors are able to diagnose MS earlier than before, and options for treatment are improving all the time. MS is a life-altering diagnosis, but because the disease is so variable, it’s impossible to predict its course. Many people, including me, live active and fulfilling lives, despite MS.
For more information about MS, visit www.msfocus.org. The Multiple Sclerosis Foundation (MSF) is a service-based, nonprofit organization dedicated to helping people with MS maintain their health and well-being. The MSF is located in Fort Lauderdale, Florida, but they’ve got ambassadors all around the country, ready to answer your questions or address your group. I’m an MSF Ambassador in Virginia and welcome comments and questions. Email me: writer@webcampone.com.
Related Reading
5 Tips for Living with MS
The Disabilities You Don’t See
No More Secs! Living, Laughing & Loving Despite Multiple Sclerosis